A Q&A with Ketogenic Dietitian Stacey Bessone, RDN, LDN. For more posts in our “Ask the Keto Dietitian” series, click here.
Can you tell us a little about yourself and your work as a ketogenic dietitian?
I am originally from Tampa, Florida and came back after finishing my education in Miami at Florida International University. I have always worked in pediatrics for my almost 24 years as a registered dietitian. I worked in the same children’s hospital I work in now right out of school but left and came back in 2011 when I took a position to exclusively practice with the medical ketogenic diet. We developed our clinic and see patients from all over the state. We also do clinical research so we can study different aspects of the diet. About half of my patients are on the classical medical ketogenic diet and the other half are on the modified Atkins® diet (MAD). I enjoy teaching the modified Atkins® diet as it is outpatient and usually with adolescents. I enjoy my job immensely and would never choose to do anything other than the medical ketogenic diet. It is so rewarding and I have the best patients and families.
How long have you been a ketogenic dietitian?
I have practiced the medical ketogenic diet exclusively for the last nine years.
How many patients do you have on the medical ketogenic diet?
We usually have between 60 and 80 patients on one of the medical ketogenic diets at a time. Often we are teaching new patients while other patients may be weaning the diet.
What is the modified Atkins® diet (MAD) for intractable epilepsy?
The modified Atkins® diet for epilepsy is a carbohydrate-controlled diet in which a patient counts carbs (minus fiber) and is encouraged to eat more fat to promote ketosis. It is started as an outpatient (meaning the patient doesn’t need to stay in the hospital) and is simpler to begin than the classic medical ketogenic diet.
How is the MAD different from the classical medical ketogenic diet for epilepsy?
The MAD diet is different in that food is measured in household measurements like tablespoons and cups or by servings (versus using a gram scale for the classical medical ketogenic diet). Instead of focusing on the ketogenic ratio (as with the classical medical ketogenic diet), the focus is on counting carbohydrates throughout the day. Fat is encouraged to be added at every meal and snack. There is no restriction on protein intake or foods with no carbohydrate. Patients learn to read food labels and can eat out at restaurants. It is a great option for adolescents and families that are on-the-go.
What types of patients are good candidates for the MAD?
Your healthcare professional will work with you to select the most appropriate diet option for your needs. In general, the modified Atkins® diet can be a suitable option for older children, teens, and adults who may find a restrictive diet more challenging. Also, MAD is a good option for patients that need diet intervention immediately and may not be able to wait for a hospital admission to do the classical medical ketogenic diet.
While not appropriate for all situations, the MAD can have a similar effect on seizure control as the classical ketogenic diet for some individuals. Most of the research shows that nearly 50% of patients on MAD have about a 50% or more reduction in seizures.
About what percentage of your keto patients are on the MAD?
About half of my patients are on the MAD.
How did the MAD come about? When was it started? Where did the idea come from?
In 2003, Dr. Eric Kossoff, a neurologist at Johns Hopkins Medicine in Baltimore, developed the novel form of the medical ketogenic diet after a patient on a classical medical ketogenic diet came for a follow up visit and had not been weighing his food and had been following the diet “loosely”. Surprisingly, the child was still in ketosis and doing very well. Following that patient, there was a young girl who was started on the Atkins® diet in advance of starting the classical diet and achieved ketosis with seizures stopping after three days. These patients had good seizure control so Dr. Kossoff investigated the less strict “modified Atkins® diet” with a formal study. He found that it was a viable option to manage epilepsy with similar results to the classical medical ketogenic diet. I am happy to be part of the research team at Johns Hopkins with Dr. Kossoff (and dietitian Zahava Turner, RD, CSP, LD) for the past several years through my hospital’s partnership with Johns Hopkins Baltimore.
What are the biggest challenges for your patients following the MAD?
The biggest challenge for patients on MAD (or any other medical ketogenic diet) is sticking to the carb count and not eating any foods that are not allowed. It can also be challenging for some patients to get enough fat. For some patients, a slip-up can lead to breakthrough seizures since the diet is helping to manage the seizures.
Is there any research on using KetoCal® with the MAD?
Yes. There was a study in 2011 in children that found using KetoCal with the MAD increased both fat intake and the ketogenic ratio (1.8:1) in comparison with MAD alone (1.01:1). A follow-up study in adults in 2018 showed that starting the MAD diet using KetoCal during the first month in a randomized protocol had better long term compliance and higher fat intake compared to those who did not use the formula.
– Stacey
Thank you, Stacey, for your insights about the modified Atkins® diet for epilepsy!
Hear from patients who have tried the modified Atkins® diet:
Looking for a hospital or program that offers the medical ketogenic diet or modified Atkins® diet? Click here to find one near you.
Learn more about the medical ketogenic diet or modified Atkins® diet for epilepsy here.
Atkins® is a trademark of Atkins® Nutritionals, Inc and not affiliated or endorsed by Nutricia North America.
I was paid by Nutricia for my time to write this blog post, however, my opinions are my own.
KetoCal is a medical food for the dietary management of intractable epilepsy and is intended for use under medical supervision. Talk with your healthcare provider to determine if KetoCal is right for you.


 Follow
Follow
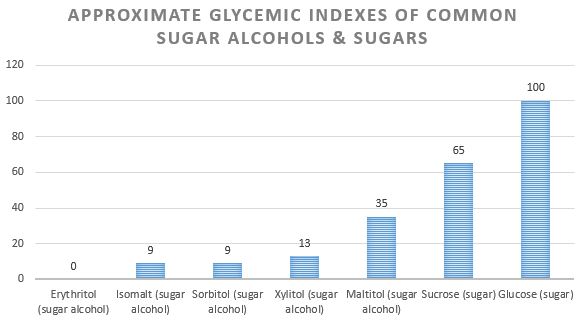
 Sugar alcohols are a specific type of carbohydrate called “polyols”. Sugar alcohols are naturally occurring in fruits and vegetables and often added to foods as a reduced-calorie alternative to sugar. Some common sugar alcohols you may see in food ingredient lists include:
Sugar alcohols are a specific type of carbohydrate called “polyols”. Sugar alcohols are naturally occurring in fruits and vegetables and often added to foods as a reduced-calorie alternative to sugar. Some common sugar alcohols you may see in food ingredient lists include: